
As we all know, the most successful and most effective fertility treatment is IVF or ICSI. It is available practically everywhere in the globe since the past 40 years or more. But even after all these years and millions of IVF cycles later, success rate is 40 to 45 percent for a woman whose age is less than 30 years. Why is that? That's because this is how far science could take us. No matter what we do, what we know about human body is just a drop of water in an ocean. Whatever medicines and techniques we use, it can only help us this much. We cannot compete with God. But this doesn't mean that the remaining 55 to 60 percent of people will never conceive. It just means that they may require more cycles, more eggs, more embryos, or other treatment modalities like PGTA, ERA, PRP, lifestyle changes or maybe donor gametes as well. This can help them further.
What do we do in an IVF cycle?
In IVF, mature eggs are removed from the ovaries, fertilised in a lab using sperm. The fertilised egg or eggs are then transported to a uterus. This if done continuously, like if we do the stimulation, do the egg pickup and then do a fresh embryo transfer, everything is usually completed within two to three weeks. But when they're done separately, like we do egg pickup and then freeze the embryos and plan embryo transfer in the next cycle, it can sometimes take longer. So, there is a lot of significant emotional, physical, and financial torque that goes with this infertility treatment. And of course, more in case of IVF because the financial burden is much higher and the number of medicines, injections all cause a lot of stress.
So, if there are some factors which can help us improve the outcome, it is always a good idea to get this identified and treated so that you get a better outcome. So let's talk about some factors which can influence the outcome.
- The first and foremost would always be age irrespective of woman or a man.
A woman is born with all the oocytes she will ever have. Out of these, only 400 to 500 will ovulate. One should remember that the biological clock will wait for no one. After the age of 35, the chances of natural conception come down. And there is also an increased possibility of chromosomal anomalies in the offspring. 24 to 35 years is the age where a woman has a highest success at having a pregnancy. Once the age crosses 35, the success reduces. Once you cross 40, the success drops further. And when you come to the number of eggs which are required to give you a successful outcome, again this also changes depending on your age. If the age is less than 30, 8 to 10 good quality mature eggs will give you around 80% chance of a live birth. When the age is between 30 to 35 years, 10 to 15 eggs are required. When you are between 35 to 37, 15 to 20 eggs are required. Once you cross 38, more than 20 eggs are required to give you a good chance at live birth. This is because as the age increases, the egg quality comes down. There may be genetic issues, there may be chromosomal anomalies in the egg which can result in giving you a poor-quality embryo. This reduces your chance at conception. This increases your chance at miscarriage as well. From this, we can see that as the age increases, you may require more than one IVF cycle to give you a good chance at pregnancy.
So, age is one factor which will always play a crucial role in the success of an IVF cycle. Of course, the same stands true even for men as well because as the age increases, DFI can increase. DFI is DNA Fragmentation Index. This signifies the quality of the sperm. If the DFI is high, the chance of getting a poor-quality embryo increases. The chances of getting a miscarriage after conception increases.
- Then comes the quality of the egg, sperm, and the embryos.
Again, age is one factor which will have an extreme impact on the quality of the egg. After this come other factors like PCOD because in PCOD, there are more follicles in the ovary.
So, these people tend to stimulate more. So, there are multiple follicles which are growing at a time. This can sometimes give you poor quality oocytes and hence poor-quality embryos as well. So, if you had like 20-25 oocytes retrieved, the number of blasts you will get on day 5 might be much less than what compared to the number of oocytes retrieved.
- Endometriosis
Endometriosis as we all know is a chronic inflammatory condition which affects almost every organ in the reproductive system. It can affect the uterus. It can cause; there may be adenomyosis. This can lead to inflammation in the uterus. This can cause chronic endometritis. This can cause, endometriosis can result in hydrosalping in the tubes. It can affect the ovary position. The endometrioma may cause difficulty in aspirating the follicles. In some people, this can even affect the quality of the egg.
- Poor ovarian reserve.
So again, poor ovarian reserve, even if there is poor ovarian reserve, if the age is young, the chances of conceiving is much better. So, if you are somebody who is ages 25 with poor ovarian reserve, you still have a very good chance of conception when compared to somebody whose age is more than 35.
- Chronic stress.
When you have chronic stress, this can also impact the quality of the oocyte.
- Sedentary lifestyle. Extreme exercise.
Obesity when the BMI is more than 25. Low BMI when the BMI is less than 18.
- Lack of sleep.
Less than 7 hours of sleep. Odd working hours. Prolonged working hours.
- Excessive caffeine intake. Smoking. Alcohol consumption.
- High junk food intake. All of this can impact your 4TT outcome.
Now let's talk about the sperm quality.
Age again is something which can make a difference like we were talking before as well because with age, the DFI can increase. DFI is a very simple test, non-invasive test where this semen sample is collected just as in a semen analysis. Then these sperms are subjected to certain tests which will give us an idea about the integrity of the DNA inside the sperm.
If your DFI is high, it doesn't mean that there is some genetic anomaly in the sperm. It just means that the genes, the chromosomal material in the sperm is fragile. So, when this chromosomal matter is given to the embryo once the fertilisation happens, the embryo also has fragile genetic material. This will impair its capacity to grow further. So, when there is high DFI, we do see a lot of miscarriages.
- Obesity
When there are obesity and the thighs are very thick, this can increase the temperature in the scrotum. High temperatures in the scrotum will affect the testis and affect the count, motility, morphology, everything because we all know the testis must be at a cooler temperature. That is the whole reason why the scrotum has a testis outside the body. But when the temperature between the legs increases because of thick thighs, this can directly impact the testis. Again, the diet you take, heat exposure, varicocele, smoking, alcohol, drugs, caffeine, this can all affect the sperm quality.
- Embryo quality
If the egg and sperm quality is good, there is a very good chance of getting a good quality embryo. Whenever we see a poor-quality embryo, we always need to go back and investigate further to find out where exactly is the issue. We see multiple, many people who come back with failed IVF cycles, one cycle, two cycle at outside centres with poor quality embryos. In these cases, it is always a good idea to look back, do all investigation, investigate the male partner also completely to see where, if there are any certain factors which can be improved. Because if the egg is good and the sperm is good, there is a very good chance of getting a good quality embryo.
- Infections in the semen.
What we see in semen analysis is just the outer issue. How the sperm looks. We don't know if there is any infection. Sometimes mild infections are not caught in semen analysis. There may not be any pustules. But when we do a semen culture, many times we see that there is a growth. Treating these infections will give you a better-quality sperm and thus a better-quality embryo. Same is the story with the varicocele. For some people, there is absolutely no issue anywhere, but they may still have DFI, high DFI. In such cases also, the embryo may be of poor quality. Taking care of this high DFI can again increase your chances of getting a good quality embryo. And when the embryo is of good quality, there is higher IVF success rates.
Then comes like other problems like fibroids, adenomyosis, hydrosalpinx, polyps, endometritis, thin endometrium, endometrial adhesions, PID, all of these factors can have an impact on the success outcome. Not all fibroids need to be removed, but if there are multiple fibroids, which is increasing the volume of the uterus, it may have an impact on the implantation. If implants also, sometimes it can lead to miscarriage. Submucosal fibroids always have to be removed.
- Adenomyosis.
Adenomyosis is something a lot more difficult to treat when compared to fibroids. For some people, it may be localised and may look like a fibroid. And if they are much farther from the uterine lining, usually we do see better outcomes than we see in a global adenomyosis where the entire volume of the uterus is very high.
- Hydrosalpinx.
Hydrosalpinx usually needs to be clicked or removed before you go for an embryo transfer. Endometrial polyps can impact the blood supply to the embryo and occupies the space in the endometrium. Small polyps, sometimes we do see that the pregnancy continues normally without any hindrance, but for some people, depending on the location of the polyp, if it is of a large size and at the fundus, this can cause a miscarriage. So endometrial polyps also have to be dealt with before you go for an embryo transfer.
- Endometritis.
Endometritis is infection inside the uterus. When the endometrium, which is the layer inside the uterine cavity gets infection, it is called as endometritis. This can impact the implantation of the endometrium and cause recurrent pregnancy loss. Thin endometrium, because of multiple causes, can impact. 7 to 14 mm is an ideal size of the endometrium when we are planning an embryo transfer.
- Endometrial adhesions.
When there are adhesions inside the uterine cavity, could be because of some infection, could be because of instrumentation like DNC. For some people, there is something called as Asherman, where the entire uterine cavity is obliterated and there is basically nothing else growing inside. In such cases, of course, we need to restore the entire uterine cavity before we go ahead and plan the embryo transfer.
- PID is Pelvic Inflammatory Disease, where there is infection in the tubes, ovaries, it could be in the peritoneum. A good course of antibiotics must be given before we plan our IVF or embryo transfer cycles. So, treating accordingly will help in improving the chances of success.
- Protocol.
What drugs we give, what dosage we'll give will also influence the number of eggs retrieved. As every person is different, so should be their treatment. One glove can't fit all. Individualised protocols, depending on the patient factors, will always help in getting better eggs. Then comes endometrium. This is one important factor which we always look at before we plan an embryo transfer cycle. When we look at the endometrium, we look at the thickness, the pattern and the vascularity. Vascularity is the blood supply to the endometrium which we can see on ultrasound. All this together plays an important role in the helping in the implantation of the embryo.
- Uterine receptivity.
Endometrial receptivity plays a crucial role in the establishment of healthy pregnancy. So, what is this endometrial receptivity? It is the ability of the endometrium to successfully attach the blastocyst to nourish it and keep it alive. For some people, this may be altered. Even though the endometrial thickness is good, the vascularity is good, the pattern is good, if the implantation window has shifted, the embryo can't attach. Then it will be a failed cycle.
IRA is an endometrial receptivity array test which helps in pinpointing the best time to transfer the embryo. In this test, the preparation of the endometrium is almost same as your embryo transfer preparation. Then instead of doing an embryo transfer, we take a biopsy, we take a small piece of endometrium and send it for testing.
They will study multiple genes and tell us which is the best time to transfer the embryo. It could be pre-receptive, receptive, or post-receptive. If it is pre-receptive, it means the endometrium is not ready to accept the embryo. So, we need to wait for a few more hours before we can do the embryo transfer. Post-receptive, it means the endometrium has passed the stage of implantation. In such cases, we must do the embryo transfer prior to the scheduled one.
So, we basically get the number of hours at which the embryo transfer must be done in the same report. Then comes the procedure of embryo transfer. Easy transfer is always preferred because we do not want to agitate the uterus, we don't want to instigate uterine contractions because this can cause expulsion of the embryo.
For people with difficult entry, contractions of uterus, fibroids, adenomyomas etc, giving a uterine relaxant prior to the ET can help to a certain extent.
The article argues that IVF success rates are influenced by a complex of interrelated variables that include age, gamete quality, uterine receptivity, lifestyle, individualized stimulation protocols, and sophisticated adjuncts such as DNA fragmentation index (DFI) analysis, PGT-A, and endometrial receptivity analysis. This is exactly where Medline Academics plays a crucial role in offering online fellowship courses in infertility. By focusing on evidence-based and clinically relevant education, Medline Academics helps fertility professionals attain a higher level of understanding that IVF success cannot be tied to a universal, “one-size-fits-all” approach. Through systematic education in Fellowship in Infertility on individualized stimulation protocols, embryo analysis, male and female factor analysis, and implantation optimization, Medline Academics bridges the theoretical gap between IVF success rates and real-world outcomes, allowing fertility professionals to make informed decisions that have the potential to positively impact patient success rates across multiple cycles.
- Lifestyle factors.
What can be done to improve the quality of the egg or the sperm? Higher mono-unsaturated fats, vegetable protein over animal protein, high fat dairy, low glycaemic index food, increased intake of iron and multivitamins, more vegetables, and fruits in the diet, at least 8 hours of sleep, moderate exercise can all do miracles in improving your reproductive health.
At Dr. Kamini Rao Hospitals, treatment is based on a careful assessment of the factors of age, egg and sperm quality, embryo development, uterine receptiveness, and lifestyle factors, rather than a standardized approach. By integrating cutting-edge technologies such as DFI evaluation, endometrial receptivity analysis, and individualized stimulation protocols by this IVF clinic in Bangalore, the goal is to maximize each step of the IVF process. This allows for the integration of scientific knowledge with practical results, increasing the potential for success while keeping patient safety and long-term reproductive well-being as the top priority.
We should always take care of your reproductive health as much as we care for our physical and mental health. All of these must go hand in hand to improve your chances at success. If your first embryo transfer is failed, it doesn't mean that you can't ever conceive. It just means that you may require more help like a different procedure or more embryos or better embryos to get a pregnancy.
Powered by Froala Editor
You may also like
More from this category.

Best Orthodontist in Lahore for Bright Smile

Couples Massage: A Relaxing Shared Experience for Body & Mind
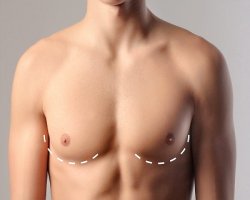
Discover Safe and Effective Gynecomastia Surgery Solutions in Riyadh

Self-Care for Moms: Breastfeeding Massage to Reduce Pain and Swelling

How Muscle Weakness Leads to Joint Damage

Why Riyadh Residents Choose Liposuction for Lasting Contours

The Role of Fermentation in Commercial Pizza Dough

Presgera USA Explained: How It Works, Benefits, and Safety Details

How to Choose Authentic Herpafend USA?

